Has Your Doctor Talked To You About Climate Change?

Dr. Mary Rice walks with Michael Howard at a Beth Israel Deaconess HealthCare clinic in Chealsea, Mass, as they test his oxygen levels with the addition of oxygen from a portable tank. He has COPD, a progressive lung disease that can be exacerbated by heat and humidity.
Jesse Costa/WBUR
hide caption
toggle caption
Jesse Costa/WBUR
When Michael Howard arrives for a checkup with his lung specialist, he’s worried about how his body will cope with the heat and humidity of a Boston summer.
“I lived in Florida for 14 years and I moved back because the humidity was just too much,” Howard tells pulmonologist Mary Rice, as he settles into an exam room chair at a Beth Israel Deaconess HealthCare clinic.
Howard, who is 57, has COPD, a progressive lung disease that can be exacerbated by heat and humidity. Even inside a comfortable, climate-controlled room, his oxygen levels worry Rice. Howard reluctantly agrees to try using portable oxygen. He’s resigned to wearing the clear plastic tubes looped over his ears and inserted in his nostrils. He assures Rice he has an air conditioner and will stay inside on really hot days. The doctor and patient agree that Howard should take his walks in the evenings to be sure that he gets enough exercise without overheating.
Then Howard turns to Rice with a question she didn’t encounter in medical school: “Can I ask you: Last summer, why was it so hot?”
Rice, who studies air pollution, is ready.

Rice, who studies the health effects of air pollution, talks with Howard about his increased breathing problems and their possible link to the heat waves, increased pollen and longer allergy seasons associated with climate change.
Jesse Costa/WBUR
hide caption
toggle caption
Jesse Costa/WBUR
“The overall trend of the hotter summers that we’re seeing [is] due to climate change,” Rice says, “and with the overall upward trend, we’ve got the consequences of climate change.”
For Rice, connecting those consequences — heat waves, more pollen, longer allergy seasons — to her patients’ health is becoming routine. She is among a very small but growing number of doctors and nurses who discuss those connections with patients.
In June, the American Medical Association, American Academy of Pediatrics and American Heart Association were among 70 medical and public health groups that issued a call to action asking the U.S. government, business and leaders to recognize climate change as a health emergency.
“The health, safety and wellbeing of millions of people in the U.S. have already been harmed by human-caused climate change, and health risks in the future are dire without urgent action to fight climate change,” the coalition statement said.
The World Health Organization calls climate change “the greatest health challenge of the 21st century,” and a dozen U.S. medical societies urge action to limit global warming.
Some societies provide patient handouts that explain related health risks. But none have guidelines that explain how providers should talk to patients about climate change. There is no concrete list of “dos” — as in wear a seat belt, use sunscreen, and get exercise — or “don’ts” — as in don’t smoke, don’t drink too much and don’t text while driving.
Climate change is different, says Rice, because an individual patient can’t prevent it. So Rice focuses on steps her patients can take to cope with the consequences of heatwaves, more potent pollen and a longer allergy season.
That’s Mary Heafy’s main complaint. The 64-year-old has asthma that is worse during the allergy season. During her appointment with Rice, Heafy wants to discuss whether she’s on the right medications. But she also wants to know why her eyes and nose are running and her chest is tight for longer periods every year.
“It feels like once [the allergy season] starts in the springtime, it doesn’t end until there’s a killing frost,” Heafy tells Rice, with some exasperation.

Rice checks Mary Heafy’s breathing during a checkup for her asthma at the Beth Israel Deaconess clinic. Climate change does seem to be extending the Boston region’s ragweed season, Rice tells Heafy.
Jesse Costa/WBUR
hide caption
toggle caption
Jesse Costa/WBUR
“Yes,” Rice nods, “because of global warming, the plants are flowering earlier in the spring. After hot summers, the trees are releasing more pollen the following season. And the ragweed — it’s extending longer into the fall.”
So Heafy may need stronger medicines and more air filters, her doctor says, and may spend more days wearing a mask — although the effort of breathing through a mask is hard on her lungs as well.
As she and the doctor finalize a prescription plan, Heafy observes that “physicians talk about things like smoking, but I don’t know that every physician talks about the environmental impact.”
There are many reasons few do. Besides the lack of guidelines, doctors say they don’t have time during a 15- to 20-minute visit to approach something as complicated as climate change.
And the topic can be controversial: While a recent Pew Research Center poll found that 59% of Americans think climate change affects their local community “a great deal or some,” only 31% say it affects them personally, and views vary widely by political party.
We contacted energy-industry trade groups to ask what role — if any — medical providers should have in the climate change conversation, but neither the American Petroleum Institute nor the American Fuel and Petroleum Manufacturers returned calls or email requests for comment.
Some doctors worry about challenging a patient’s beliefs on the sometimes-fraught topic, according to Dr. Nitin Damle, the past president of the American College of Physicians.
“It’s a difficult conversation to have,” says Damle, who practices internal medicine in Wakefield, R. I. . “Many people still think it’s something they’re not going to be affected by, but it’s really not true.”
Damle says he “takes the temperature” of patients, with some general questions about the environment or the weather, before deciding if he’ll suggest that climate change is affecting their health.
Gaurab Basu, a primary care physician at Cambridge Health Alliance, says he’s ready if patients want to talk about climate change, but he doesn’t bring it up. Basu says he must make sure patients feel safe in the exam room. Raising a controversial political issue might erode that feeling. When patients do ask about climate change, it can be “a difficult conversation,” he says.
“I have to be honest about the science and the threat that is there, and it is quite alarming,” Basu says.
So alarming that Basu says he often refers patients to counseling. Psychiatrists concerned about the effects of climate change on mental health say there are no standards of care in their profession yet. They suggest a response must be tailored for each patient, but some common responses are emerging.
“We Are Hungry for Information”
One environmental group isn’t waiting for doctors and nurses to figure how to talk to patients about climate change.
“We’re trying to create a demand for these conversations to get started,” says Molly Rauch, the public health policy director with Moms Clean Air Force, a project of the Environmental Defense Fund.
Rauch urges the group’s more than one million members to ask doctors and nurses for guidance. For example: When should parents keep children indoors because the outdoor air is too dirty?
“This isn’t too scary for us to hear about,” Rauch says. “We are hungry for information about this, we want to know.”
But Rauch says it doesn’t seem like climate change is breaking into the medical community as a health issue. One study found classes about environmental health or global warming at only 20 out of 140 U.S. medical schools.
A few nursing schools are adding climate-related courses to their training, to prepare students for conversations with patients.
“Nurses need to catch up quickly,” says Patrice Nicholas, director of the Center for Climate Change, Climate Justice and Health at the MGH Institute of Health Professions in Boston.
Nicholas attributes the delay, in part, to politics. “Climate change really needs to be reframed as a public health issue,” Nicholas says.
The few doctors and nurses who have started discussing climate change with their patients say they’ve not had much pushback, but that may be because bringing climate change into the exam room is still very new.
This story is part of NPR’s reporting partnership with WBUR and Kaiser Health News, an editorially independent news service of the Kaiser Family Foundation.
Overhauling Kidney Care
This week, President Trump signed an executive order aimed at improving the care of kidney patients. Nephrologist Amaka Eneanya talks with Scott Simon about some of the new initiatives.
SCOTT SIMON, HOST:
Americans with kidney disease got some encouraging news when President Trump signed an executive order aimed at improving their care.
(SOUNDBITE OF ARCHIVED RECORDING)
PRESIDENT DONALD TRUMP: Those who suffer from kidney disease experience a significant toll on their daily lives.
SIMON: The administration wants to improve detection and diagnosis, increase the number of kidney transplants and move patients away from commercial dialysis centers by encouraging more in-home dialysis. Medicare now spends about $114 billion on kidney care every year, about a third of that on people who need regular dialysis or a transplant.
Dr. Amaka Eneanya is a nephrologist with Penn Medicine at the University of Pennsylvania. She treats patients with chronic kidney disease. Thanks very much for being with us.
AMAKA ENEANYA: Thank you for having me on, Scott.
SIMON: The scope of kidney illness in this country is enormous, isn’t it?
ENEANYA: That’s correct. So approximately 37 million adults have chronic kidney disease in United States. And the majority of those adults are unaware of their diagnosis, upwards of 90%.
SIMON: One of the proposals, and certainly one that a lot of people noticed, is encouraging patients to have dialysis at home…
ENEANYA: That’s correct.
SIMON: …Which I gather is common in some countries around the world, but not the United States. Why not so far?
ENEANYA: So there’s a few reasons for that. So one, the training for clinicians who actually do provide care for patients with kidney disease is not very robust for home dialysis. Also, the payment incentives, as they are now, really favor doing dialysis in in-center dialysis facilities. Also, education for patients is still evolving for them to learn about home dialysis.
SIMON: How do you do home dialysis?
ENEANYA: Basically, what your kidneys do is to, on a regular, you know, 24/7 basis, clean the body of fluid and waste. And that’s basically what your urine is. And so when you’re doing home dialysis, you have machines that are actually doing this for you. So you’re connecting to this machine, and it’s removing fluid and waste from the body, just as your kidneys would do.
SIMON: And this works overseas?
ENEANYA: This works incredibly well. Countries – Guatemala, Mexico, Hong Kong have the majority of their patients using some type of home dialysis.
SIMON: I noticed some medical sources this week, in response to the president’s plan, said, look; what we have is working now. Why endanger that?
ENEANYA: The question is who is it working for? If it’s working for the patients and we have a resounding response from them that that’s what the case is, then by all means, we should reconsider and look at things very closely. But that’s not what research has shown, and that’s not what my experience has been, and many others, in terms of caring for these patients. It’s quite a burden to do things the way that they have been doing, which is most of the patients going to dialysis or receiving their dialysis in a facility.
SIMON: The administration wants to double the number of kidneys available for transplant. How do you do that?
ENEANYA: Part of what he was describing was incentivizing donors – paying them for lost wages and child care that they may have to use after doing a surgery. I think a lot of the time, there’s a focus on the recipient because they have this chronic disease, and they’re getting a fresh, new kidney, and great for them. But I recently had an experience where I spoke to a altruistic donor, so a person who just decided to donate a kidney out of the goodness of their heart. And she really remarked, you know, tearfully, how difficult the post-operative period was and how she really wasn’t prepared for how long she would be…
SIMON: Yeah.
ENEANYA: …Out of work and, you know, how difficult that was. And so I think actually educating donors and providing these incentives will really make a difference.
SIMON: Do you think the executive order signed this week is going to – has the hope of improving life for kidney patients in a couple of years?
ENEANYA: Absolutely. This was a phenomenal kind of monumental time for the field of nephrology and for patients with kidney disease. If the goal is to have 80% of patients with end-stage kidney disease to be on a home dialysis modality or to receive a transplant, that’s a really big change. And so we know that quality of life will be – will improve. Patients will have kind of more choices in terms of what is best for them. It’s really an exciting time.
SIMON: Dr. Amaka Eneanya, a nephrologist with Penn Medicine, University of Pennsylvania. Thanks so much for being with us.
ENEANYA: Thank you so much.
(SOUNDBITE OF MUSIC)
Copyright © 2019 NPR. All rights reserved. Visit our website terms of use and permissions pages at www.npr.org for further information.
NPR transcripts are created on a rush deadline by Verb8tm, Inc., an NPR contractor, and produced using a proprietary transcription process developed with NPR. This text may not be in its final form and may be updated or revised in the future. Accuracy and availability may vary. The authoritative record of NPR’s programming is the audio record.
A Call For More Research On Cancer’s Environmental Triggers
A stretch of the Mississippi River from New Orleans to Baton Rouge, La., that is crowded with chemical plants has been called “Cancer Alley” because of the health problems there.
Giles Clarke/Getty Images
hide caption
toggle caption
Giles Clarke/Getty Images
We already know how to stop many cancers before they start, scientists say. But there’s a lot more work to be done.
“Around half of cancers could be prevented,” said Christopher Wild in the opening session of an international scientific meeting on cancer’s environmental causes held in June. Wild is the former director of the World Health Organization’s International Agency for Research on Cancer.
“Cancer biology and treatment is where most of the money goes,” he said, but prevention warrants greater attention. “I’m not saying that we shouldn’t work to improve treatment, but we haven’t balanced it properly.”
Perhaps no question about cancer is more contentious than its causes. People wonder, and scientists debate, if most malignancies stem from random DNA mutations and other chance events or from exposure to carcinogens, or from behaviors that might be avoided.
At the conference in Charlotte, N.C., scientists pressed for a reassessment of the role of environmental exposures by applying modern molecular techniques to toxicology. They called for more aggressive collection of examples of human pathology and environmental samples, including water and air, so that cellular responses to chemicals can be elucidated.
The hope is that by identifying specific traces of exposures in human cancer specimens, scientists can identify environmental causes of disease that might be prevented.
“Over 80,000 chemicals are used in the United States, but only a few have been tested for carcinogenic activity,” said Margaret Kripke, an immunologist and professor emeritus at MD Anderson Cancer Center, in an interview at the meeting.
“This has been a very neglected area of cancer research for the last several decades,” said Kripke, the driving force behind the conference, which was put on by the American Association for Cancer Research. “Environmental toxicology was very popular in the 1950s and 1960s,” she said, but genetics then began to overshadow studies of cancer’s environmental causes. “Toxicology fell by the wayside.”
While the incidence of tobacco-linked cancers has been falling, malignancies not associated with smoking are rising, Kripke said. Recent evidence suggests an escalating rate of lung cancer in nonsmokers. That trend implicates other environmental factors.
Around the globe, cancer’s overall incidence is climbing. This year, 18 million people will be diagnosed with some form of cancer and over 9 million will die from it.
Infections — many preventable, such as by human papillomavirus —account for 15% of new cases.
Another rising cause is obesity, along with urbanization. People generally get less physical activity and eat differently in cities, and pollution is heavier there, too. “As people move into cities, that will drive up cancer rates,” Wild said.
One of the biggest obstacles to preventing cancer is that many people just don’t think it’s feasible. Progress “requires long-term vision and commitment,” Wild said. “Funding is limited, and there’s little private sector investment.”
A change in the way benefits of cancer prevention are framed could help. “When I was at the IARC, one thing that struck me was the power of economic arguments over health arguments for preventing cancer,” Wild said.
Cancer treatment costs can be prohibitive. But productivity lost from premature deaths in Brazil, Russia, India, China and South Africa alone runs $46.3 Abillion annually, he said. “Developing countries are not prepared to deal with the rising cancer burden.”
The precise proportion of cancers arising from environmental and occupational exposure to carcinogens is uncertain. In 2009, a report by the President’s Cancer Panel called prior approximations of around 6% “woefully out of date” and low. A 2015 paper by over a hundred concerned scientists cited “credible” estimates of 7% to 19%.
Scientist at the Charlotte meeting emphasized the complexity of cancer’s causes and the need for toxicologists to update methods to reflect that complexity, such as by studying interactions of environmental and genetic risks, and by examining cells after a mix of exposures. “Most toxic exposures do not occur singly,” said Rick Woychik, deputy director of the National Institute of Environmental Health Sciences.
Until recently, many toxicology tests were performed in rodents, because it would be unethical to deliberately evaluate possible carcinogens in people. But these animal experiments are labor-intensive and slow, he said.
New alternatives are now being tried. “We learned from pharma that with robotics and high-throughput technology you can interrogate a lot of biology quickly and at lower costs,” he said.
Epidemiological research of human exposures has been stymied by the difficulty of proving cause-and-effect — that a particular substance actually causes cancer — and by shortcomings of survey data from questionnaires.
At the conference, scientists offered glimpses of new technology that is helping fill informational gaps.
Bogdan Fedeles of MIT explained how DNA serves as a lifelong “recording device.” He and others use duplex sequencing to examine human samples for genetic “fingerprints of exposure.”
Allan Balmain, a geneticist at University of California, San Francisco, spoke about mutational signatures in malignancies. In liver cancer, for instance, these signatures can offer causal clues—such as smoking, alcohol or aflatoxin, a product of mold that grows on some foods.
Many chemicals that cause or stimulate cancer growth are produced inside our bodies. “It’s not all about the environment,” Balmain said.
Others highlighted a conceptual shift in how scientists define carcinogens. Key characteristics may include a substance’s capacity to stimulate growth of malignant cells, or to induce inflammation—without necessarily causing DNA damage, long seen as the necessary .
“The answer to ‘What is a carcinogen?’ is changing” said Ruthann Rudel, a toxicologist at the Silent Spring Institute who has published extensively on breast carcinogens. She detailed new techniques to screen breast cancer cells for changes in response to specific chemical exposures.
The public health stakes for the field are high.
Professor Polly Hoppin, of the University of Massachusetts, Lowell, discussed cancer-causing industrial contamination of drinking water at Camp Lejune, N.C., air pollution in St. John the Baptist Parish, La., and potential exposures to carcinogens from fracking and planned plastics production in Pennsylvania.
Hoppin reflected on the U.S. experience with tobacco cessation. Scientists knew that smoking causes cancer by the 1950s, she said. Implementing that knowledge required policy and incentives — like high cigarette taxes and public smoking bans — and took decades.
“The science wasn’t enough,” Hoppin said. “How many lives could have been saved if we’d acted sooner?”
Elaine Schattner is a physician in New York writing a book on cancer attitudes that will be published by Columbia University Press.
As Its Drug Pricing Plans Fall Through, Trump Administration Turns To Congress To Act

Secretary of Health and Human Services Alex Azar announced his agency is dropping a proposal intended to lower drug prices.
Michael Brochstein/SOPA Images/LightRocket via Getty Images
hide caption
toggle caption
Michael Brochstein/SOPA Images/LightRocket via Getty Images
The Trump administration has dropped one of the meatiest portions of its plan to reduce drug prices.
The Department of Health and Human Services said it will no longer pursue a rule that would have prohibited the payment of certain rebates on drugs in Medicare Part D and Medicaid plans.
The idea was to target the middlemen, pharmacy benefit managers, whose negotiations with drugmakers and insurers influence the costs consumers pay for drugs.
The hope was the rule would have effectively pressured drugmakers to give discounts to consumers instead of middlemen, HHS secretary Alex Azar said in remarks to the media in February. “Passing discounts directly on to the patient will move us toward a real market for drugs,” said Azar. “We’re going to fundamentally rewire how we pay for drugs in this system.”
Right now, if you’re a Medicare Part D beneficiary, and you need to pick up a drug that has a $120 list price, you might have to pay that full price, even if the middleman that negotiates on behalf of your insurer only pays a net price of $100 for it, after rebates. The idea of this proposal was that the consumer would only have to pay the discounted price.
When the rule was first announced, drugmakers supported the idea, and some drug pricing experts said it could be an effective move. “This is a huge potential change, transformative,” Dr. Walid Gellad, director of the Center for Pharmaceutical Policy and Prescribing at the University of Pittsburgh told NPR.
But some critics were concerned that the move wouldn’t address drugs’ list prices that are the starting point for negotiations.
Also, there was a worry that the elimination of rebates could ultimately cost seniors more, in higher premiums on their Medicare plans. The nonpartisan Congressional Budget Office in May determined the plan would cost the federal government $177 billion over nine years, largely from increases in the government’s share in the cost of premiums.
In a briefing with reporters Thursday, Azar said the administration scrapped the plan after getting feedback from the public and stakeholders. “At the end of the day, while we support the concept of getting rid of rebates, while we appreciate and are passionate about the problems and the distortions in the system caused by this opaque rebate system, we’re not going to put seniors at risk of their premiums going up.”
“Congress perhaps might even take this up — they have more tools than we do,” Azar said. “They can actually look more holistically at changes to the system that could also mitigate or protect seniors from bearing any impact of change. I don’t have those tools; they might have those tools.”
A senior Trump administration official, who spoke on background during a separate briefing Thursday, echoed those sentiments, saying their primary focus is to support a legislative deal to lower drug prices and that there was concern this change would disrupt those efforts.
Drugmakers were in favor of trying to bring consumer prices down by targeting middlemen. The drug industry trade group PhRMA called the rollback of the plan “a blow to seniors who could have paid less for their medicines at the pharmacy counter.”
“Of all the policies proposed in Washington right now, this was the only proposal that would provide immediate savings at the pharmacy counter, instead of only saving the government or insurance companies money,” said Holly Campbell, PhRMA’s deputy vice president of public affairs in a statement.
Other stakeholders cheered the administration’s reversal of the proposed rule, including groups representing private insurers, public sector health plans and pharmacy benefit managers. They pointed to the prices set by drugmakers as a better focus for efforts to reduce drug costs.
“Any solution should start with addressing drug prices,” T.J. Crawford, a spokesman for CVS Health, which operates a large pharmacy benefit manager, wrote to NPR.
Matt Eyles, president and CEO of America’s Health Insurance Plans, said in a statement: “As we all know, drug prices and price increases are set and controlled solely by drugmakers. They alone could decide to reduce prices – and can do so today.”
The rebate reversal is the second defeat for the administration on drug pricing in a week, coming just days after a court struck down another pillar of its drug pricing plans, a proposed regulation to require that drug companies disclose prices in ads.
Azar says the administration hasn’t given up on lowering drug prices. But Congress will have to play a bigger role. “We have many other things that we’re doing in drug pricing,” he says. “We are working on a bipartisan basis with Congress on drug pricing legislation.”
The White House official who briefed reporters Thursday said people in the administration don’t plan to “twiddle our thumbs” while the legislative process plays out, and are working on a number of plans.
President Trump hinted at one idea last week — a “most favored nation” clause that would tie American drug prices to what other countries pay. The administration has not released any details about how that would work or when it would roll out.
Young Undocumented Californians Cheer Promise Of Health Benefits
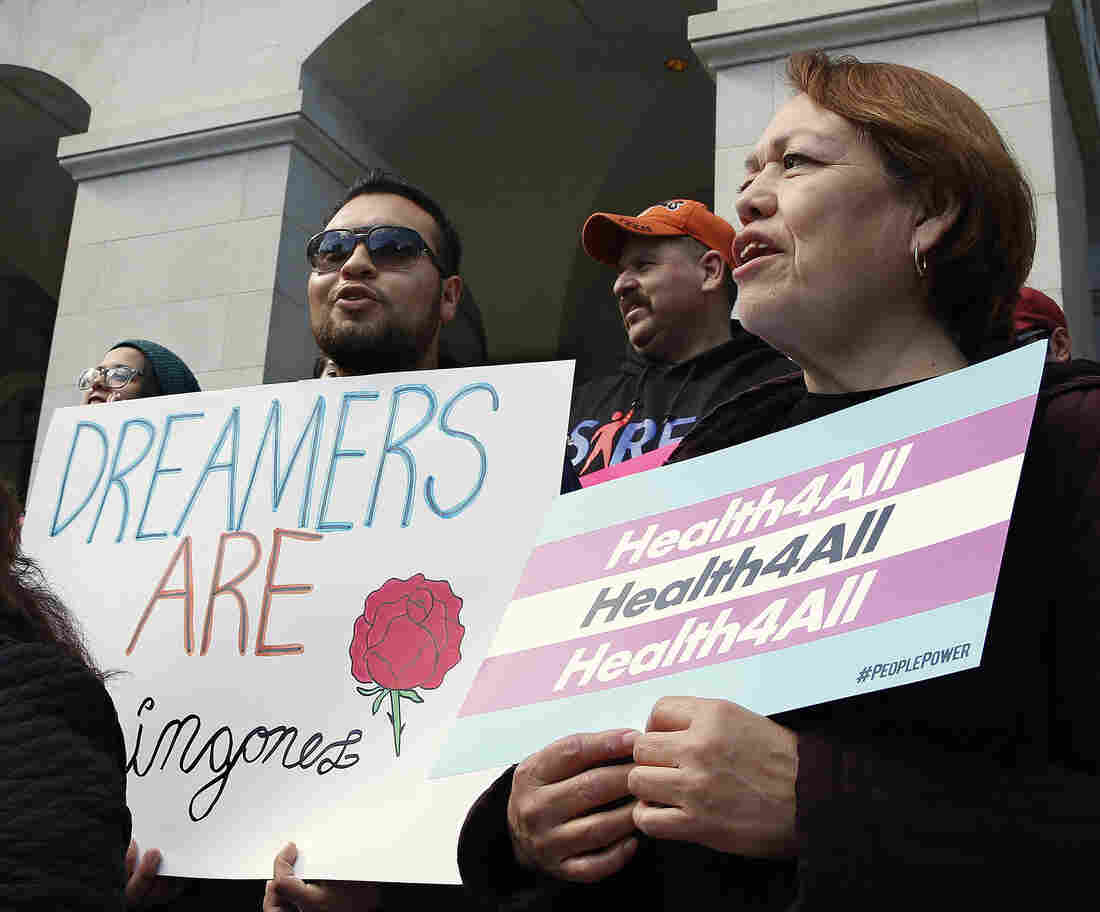
Demonstrators rallied in Sacramento in May for Medi-Cal expansion to undocumented Californians. When the state’s budget was finalized, only young adults up to age 26 were authorized to be included in the expansion. Gov. Gavin Newsom says that’s an important first step.
Rich Pedroncelli/AP
hide caption
toggle caption
Rich Pedroncelli/AP
For years, Beatriz Basurto’s family has had to make hard choices about when to pay for medical care, and who should get treatment.
“To me, it was always the doctor would be the last resort,” she says. “But for my parents, the doctor was never a choice. No matter how sick they got, they had to suck it up.”
Basurto, 19, says her parents always put the kids’ medical needs before their own. The family moved to California from Mexico more than 15 years ago. During that time, most of her family members have been ineligible for Medi-Cal, the state’s version of Medicaid, because they aren’t citizens.
Their situation started to change in 2016, when California expanded the program to all low-income children 18 and under, regardless of immigration status. That opened the doors for Basurto’s little sister to enroll.
And starting in January of 2020, Beatriz will be allowed to sign up, too.
California’s governor signed a law Tuesday that approved $98 million to expand Medi-Cal to income-eligible undocumented adults from age 19 until they turn 26, making it the first state in the United States to cover this group. California estimates 138,000 young adults will become insured under the new policy.
While the state has expanded options for children and young adults, most undocumented people in California still have limited access to health care. They can sign up for “restricted” Medi-Cal, but it only covers emergencies and pregnancy-related care. Many people on this plan end up putting off treatment or turning to county clinics for help.
Supporters who want to further expand Medi-Cal to all residents say that move would boost public health and bring down emergency room costs. California Gov. Gavin Newsom has vowed to make everyone eligible.
“We believe in universal health care,” he said during a speech this month. “Universal health care’s a right, and we’re delivering it — regardless of immigration status — to everyone up to the age of 26, and we’re gonna get the rest of that done, mark my words.”
But after months of debate at the California State Capitol, proposals to offer Medi-Cal to all undocumented adults, as well as a push to cover undocumented seniors, were deemed too costly.
Medicaid is a joint state-federal program, but California would use state dollars to pay for expanded benefits to immigrants living in the U.S. without legal permission.
Some lawmakers argued California should be spending health care dollars on its own citizens, rather than people who are not living in the state legally.
“We are going to be a magnet that is going to further attract people to a state of California that’s willing to write a blank check to anyone that wants to come here,” said state Sen. Jeff Stone, a Republican, at a recent legislative hearing.
President Donald Trump also criticized California for offering health insurance to undocumented people.
“They don’t treat their people as well as they treat illegal immigrants,” the Republican president told reporters in the White House on Monday. “It’s very unfair to our citizens and we’re going to stop it, but we may need an election to stop it.”
But advocates say California isn’t done fighting for Medicaid expansion.
Almas Sayeed, deputy director of the California Immigrant Policy Center, says providing health care is crucial, given federal anti-immigrant hostility.
“For young immigrants, it’s a moment of feeling like we don’t belong in this country,” she says. “We work really hard in California to make sure communities know that they do.”
Beatriz Basurto is eager to sign up for Medi-Cal this January. She attends community college near Los Angeles, and wants to become an environmental scientist. She hopes getting insurance will allow her to seek out mental health care for ongoing stress, some of which she attributes to hostile political rhetoric about immigrants.
“The world isn’t always so welcoming,” she says. “It can be really, really overwhelming. It exhausts you mentally. It’s almost like I have no time to feel anything, because there’s always something else I have to do.”
Brenda Huerta, an undocumented 22-year-old, was enrolled in a health plan through her university. But that coverage expired this summer, after she graduated. She says her college plan was great for checkups, but didn’t cover large expenses.
When Huerta broke her leg she ended up paying for her care out-of-pocket. And she’s still helping pay off hospital bills from when her mom had major surgery.
Huerta needs new glasses, and she wants to continue regular medical and dental care. But she isn’t sure if she’ll sign up for Medi-Cal next year. Even with coverage, she’s worried her costs will stack up.
“Paying the [student] loans that I have, I haven’t really been thinking about health insurance,” she says.
She and other young adults recently met with Gov. Gavin Newsom to lobby for the expansion of Medicaid eligibility to all Californians.
“Everyone in the room, we did talk about our struggles as undocumented people not having health insurance,” she says. “And we also mentioned how our parents suffer from not having health insurance, because it puts an economic burden on us.”
Newsom’s office estimated expanding eligibility to all undocumented adults would cost $3.4 billion. About two thirds of California’s roughly 2.2 million undocumented immigrants would qualify for Medi-Cal based on income guidelines.
Basurto says even though coverage for undocumented young adults is a small step in the larger battle for equal rights, it makes her feel more at home in the U.S.
“I do belong here,” she says, “regardless of what others say.”
This story is part of NPR’s health reporting collaboration with Capital Public Radio and Kaiser Health News.
Leaders From 13 States Urge Federal Court To Allow Supervised Injection Sites

Supplies sit on a check-in desk at a model of a hypothetical injection site in San Francisco, pictured here in September 2018. Local leaders from San Francisco are among a dozen local officials urging a federal court to allow an effort to open a supervised injection site in Philadelphia.
Eric Risberg/AP
hide caption
toggle caption
Eric Risberg/AP
Top officials from 13 states are joining Philadelphia in urging a federal court to allow a site to open where people can inject illegal opioids under medical supervision, the latest escalation in a legal battle with the Justice Department that may determine whether such facilities, known as supervised injection sites, can start to operate in America.
In Philadelphia, where drug overdoses — most involving opioids — kill three times as many people as homicides, a nonprofit called Safehouse has been working to launch an injection site as a way of combating the city’s opioid crisis.
But the Justice Department has mounted a legal challenge to block it before it opens, claiming such a site violates federal drug laws and would enable drug use.
A friend-of-the-court brief submitted Wednesday by leaders from five cities — Ithaca, New York City, Pittsburgh, San Francisco and Seattle — says injection sites, widely used in parts of Canada and Europe, need to be part of the way cities respond to the opioid crisis.
“The opioid crisis has taken a major toll on American cities and counties, including ours,” the city leaders wrote. “Despite our efforts, the existing methods of combating the opioid crisis have proven to be too little, or at least too late, for far too many of our residents.”
In a separate brief, attorneys general from Washington, D.C., and seven states including Michigan, New Mexico and Oregon also urged the court to allow the injection site to open. “As laboratories of experimentation and the primary regulators of public health, States should be free to adopt cutting-edge medical interventions,” the top state law enforcement officials wrote. The other top state law enforcement officials who signed on to the brief are from Delaware, Minnesota, Virginia and Colorado.
The opioid crisis has also resulted in an alarming death rate in the cities that are exploring injection sites like the one Philadelphia is pursuing.
In New York City alone, more than 1,000 people die every year from overdoses. “That means more New Yorkers die of opioid overdoses than from homicides, suicides and vehicle crashes combined,” the city leaders’ brief notes.
But legal uncertainty and other issues have slowed the efforts to open supervised injection sites. However, city leaders say they believe no other option is able to put a significant dent in lethal overdoses.
“These trends have continued despite extensive efforts by local governments and health departments to curb the crisis, including policies to expand medication-assisted treatment, clean needle exchanges, and the distribution of naloxone to first responders and public health workers,” the city officials wrote.
Justice Department officials have stated that the idea of a supervised injection site violates so-called crack house laws that make it a crime to own a property where drugs are being used, but Safehouse planners and an alliance of local leaders counter that statutes from the 1980s were never intended to apply to what they view as a medical facility in the midst of a public health crisis.
The city leaders write that the sites “would be places where drug users can obtain medical supervision and treatment. The act of allowing drug users to [inject drugs] in a supervised environment where they can be rescued if needed, rather than on the street or in a restroom stall.”
A barrage of other briefs were also filed to the federal court in Philadelphia on Wednesday both in support of and opposing the proposed site. Among them, one written by a group of 64 current and former law enforcement officials, including former Justice Department officials, claiming that federal prosecutors were “distorting federal drug laws” in trying to shut down the country’s first attempt at opening a supervised injection site.
But a group of six neighborhood associations around the Philadelphia neighborhood of Kensington, the heart of the city’s opioid crisis and the preferred location of the injection site, wrote a brief pleading with the court to not allow the site in their community, fearing such a facility would invite additional crime and drug trafficking.
“Law abiding citizens walking to and from work and young children traveling to school face the risk of getting caught in the violence and become targets for the dealers looking to increase their customer base,” wrote the neighborhood group, which filed the brief along with the city’s Fraternal Order of Police.
“The police, who are experts in this area, know what Congress knew. They know from bitter experiences that concentrating drug use in a place like the one that Safehouse proposes will bring more addicts, more dealers and more violent crime to neighborhoods that are already suffering,” the brief says.
Yet, the brief from the states’ attorneys generals argues that studies have shown that injection sites have proved to save lives in other countries, and that it is time for the U.S. to give the controversial measure a chance.
“States that are home to metropolitan areas should be free to experiment with this potentially lifesaving intervention, as well as others, without fear that public health nonprofits or doctors in their jurisdictions will be subject to prosecution,” the group wrote.
The case is pending in Philadelphia before U.S. District Judge Gerald A. McHugh, who will rule sometime after a July 22 filing deadline.
Trump Administration Announces Plans To Shake Up The Kidney Care Industry

President Trump signed an executive order Wednesday proposing to change how kidney disease is treated in the United States. It encourages in-home dialysis and more kidney donations.
Nicholas Kamm/AFP/Getty Images
hide caption
toggle caption
Nicholas Kamm/AFP/Getty Images
Updated 6:30 p.m.
The Trump administration has announced an ambitious plan to change treatment for kidney disease in the United States.
President Trump signed an executive order Wednesday directing the Department of Health and Human Services to develop policies addressing three goals: reducing the number of patients developing kidney failure, reducing how many Americans get dialysis treatment at dialysis centers and making more kidneys available for transplant.
“With today’s action, we’re making crucial progress on another core national priority: the fight against kidney disease,” Trump said at a speech prior to signing the order.
Kidney disease is the ninth-leading cause of death in the U.S. and a major expense for the federal government. Medicare pays for end-stage renal disease treatment, including dialysis and kidney transplant.
“Taxpayers spend more on kidney disease — over $110 billion — than we do on the National Institutes of Health, the Department of Homeland Security and NASA combined,” Joe Grogan, head of the White House’s Domestic Policy Council told reporters.
The executive order pushes for changes in three areas: prevention, dialysis care and kidney donation. To implement parts of the order, the Centers for Medicare and Medicaid Services announced Wednesday five proposed payment models intended to increase innovation in the delivery of kidney care.
Better prevention of kidney failure is desperately needed, according to Dr. Holly Mattix-Kramer, a kidney specialist at Loyola University Chicago and the president of the National Kidney Foundation. Mattix-Kramer was among dozens of kidney specialists and patient advocates who attended the announcement Wednesday.
“We’re extremely excited,” she says. “For so long we felt like no one was paying attention to this epidemic of kidney disease.”
One problem, she explains, is that there hasn’t been financial incentive to get doctors to screen for kidney disease or to diagnose and educate patients about it. “Once you get kidney failure then there’s a payment structure for that,” she says. “But there lacked a good payment structure incentive for preventing kidney failure, which seems not intuitive and seems obviously something that we should fix.”
The executive order proposes to change the way Medicare providers are paid to motivate them to focus on patient education and preventing the progression of kidney disease. It also calls for an awareness campaign. “Forty percent of Americans with some stage of kidney disease do not know they have it,” Health and Human Services secretary Alex Azar told reporters on a call Wednesday morning.
A key focus of the executive order is effort to encourage in-home dialysis. One of the new, proposed CMS models incentivizes clinicians to offer this option to patients.
Currently, most dialysis is delivered at dialysis centers, a multibillion-dollar industry dominated by two for-profit companies. In-center dialysis can be time-consuming and burdensome for patients.
“Currently only 12% of American dialysis patients receive it at home. That would compare to 56% in Guatemala and 85% in Hong Kong,” said Azar. “We want to get to 80% of those who are under treatment either in-home dialysis or transplanted eventually — so a radical change from where we stand now.”
CMS Administrator Seema Verma explained that the current system prioritizes payment to in-center dialysis, but her agency wants to start to incentivize in-home dialysis and transplants.
“The way we currently pay for chronic kidney disease and kidney failure isn’t working well for patients,” said Verma in a statement.
Mattix-Kramer says the administration’s targets for increasing the proportion of patients getting dialysis at home may be overly ambitious. “It’s great to have big goals like that, but I do think 80% is going to be incredibly difficult,” she says.
For a lot of her patients, it wouldn’t be easy to switch to in-home treatment. “You need social support and you need a clean house and you need someplace to have equipment. Many of our patients live in areas where they don’t even have a grocery store in their neighborhood,” she says. “A lot of those socioeconomic issues would need to be addressed.”
Another focus of the executive order is the organ transplant system. Currently, close to 100,000 people are on a waiting list for kidneys.
“Many, many people are dying while they wait,” Trump said, addressing a room full of kidney doctors, advocates and patients in Washington, D.C., just before signing the executive order. “We’ll do everything we can to increase the supply … of the available kidneys and getting Americans off these waitlists.”
Azar said he believes it’s possible to double the number of kidneys available for transplant by 2030. “There is currently a lack of accountability and wide variability among these organ procurement organizations,” he said. “The executive order will demand a much higher level of accountability.” He also said living donors could receive compensation from the government for lost wages and child care.
Finally, the executive order encourages research and development of an artificial kidney, an innovation that could someday replace the need for transplants.
Administration officials touted Wednesday’s news as the first major action related to kidney disease in decades. Previous administrations, including Barack Obama’s, have suggested similar initiatives, but not much has changed.
Andy Slavitt, who ran the Centers for Medicare and Medicaid Services under President Obama, praised Wednesday’s announcement on Twitter. “Care of kidney patients has been broken in the US for a long time, plagued with a corporate duopoly [and] a lower income minority population losing out,” he wrote.
But he also pointed out that as the Trump administration makes this announcement, it is arguing in court that the Affordable Care Act should be struck down as unconstitutional. “There is one law that makes this new change possible. The same law that requires people with [preexisting] conditions get coverage. The ACA,” he tweeted. “Without it, there is no authority to do this.”
It was unclear how quickly these changes could roll out. Frequently, Trump’s executive orders instruct agencies to develop federal rules, a lengthy bureaucratic process. One more immediate change is in how Medicare providers are reimbursed; CMS announced that its proposed payment models would roll out starting in January 2020.
Years After Sexual Assault, Survivors Hounded To Pay Bills For The Rape Kit Exam

For 25 years, the federal Violence Against Women Act has required any state that wants to be eligible for certain federal grants to certify that the state covers the cost of medical forensic exams for people who have been sexually assaulted.
Christian Science Monitor/Getty
hide caption
toggle caption
Christian Science Monitor/Getty
Six years ago, a newly minted graduate of the School of the Art Institute of Chicago was working three part-time jobs and adjusting to life as a non-student. She stopped in for a drink one night at a restaurant in Chicago’s Bucktown neighborhood, where she got into a conversation with a guy. The next thing she remembers clearly was awakening at home the next morning, aching, covered in bruises, with a swollen lip.
She believed she had been raped and went to the local police station to file a report. The police sent her to a hospital emergency room nearby where, with her permission, a doctor did a medical forensic exam, checking her for injuries and taking evidence from her body and clothes to potentially use in a prosecution case. The exam took hours and made her even more miserable.
Police never made an arrest.
As time passed and the woman tried to move past the assault, she received regular, unwelcome reminders: bills from the hospital and emergency physicians group that treated her.
The physicians group eventually sent her bill to a collection agency, and she started receiving nagging phone calls as well. Now 28 and living near Dallas, she still gets phone calls and letters a couple of times a year ordering her to pay up.
“When I get that phone call, it’s still so raw. I’m shaking,” says the woman, whose first name is Erin. (NPR has agreed not to use Erin’s last name, to protect her privacy.)
For 25 years, the federal Violence Against Women Act has required any state that wants to be eligible for certain federal grants to certify that the state covers the cost of medical forensic exams for people who have been sexually assaulted.
Subsequent reauthorizations of the Act have clarified that these individuals also can’t be required to participate with law enforcement to get an exam; nor do they have to pay anything out-of-pocket for that exam at any point (not even if they would be reimbursed later).
And yet for some people who have been raped, the bills keep coming — despite this long-standing federal prohibition and other state laws that provide additional financial protections in many places.
“There’s often a disconnect between the emergency room personnel that take care of the person and the billing department that sends out the bills,” says Jennifer Pierce-Weeks, CEO of the International Association of Forensic Nurses, professionals who have specialized training in how to evaluate and care for victims of violent crime or abuse.
There is wide variation in how states meet their financial obligations to cover sexual assault exams — sometimes called “rape kits” — that collect evidence of the crime. Many states tap funds they receive under the federal Victims of Crime Act. Others use money from law enforcement or prosecutors’ budgets or other designated options.
What services are covered as part of the rape exam can vary by state as well. Federal rules require that the patient be interviewed and examined for physical trauma, penetration or force, and that evidence be collected and evaluated.
But many states include additional services without charging victims, including testing and treatment for pregnancy or sexually transmitted diseases. Some may cover treatment for counseling, or for injuries that survivors experience during the assault.
Having financial protections on the books for people who have been raped, however, doesn’t necessarily translate to seamless, no-cost services on the ground.
For instance, New York requires that patients treated for sexual assault receive some services at no charge beyond the federal requirements, including emergency contraception and treatment for STDs, says Christopher Bromson, executive director of the Crime Victims Treatment Center in New York.
Still, last November the New York attorney general’s office announced settlements with seven hospitals that had illegally charged more than 200 such patients for medical forensic exams, with amounts ranging from $46 to $3,000. In some cases, the hospitals referred the individuals to bill collectors who dunned them for the payments.
Afterward, the Healthcare Association of New York State, a nonprofit group that advocates for better health services, teamed up with the state Department of Health and others to present four webinars for hospital personnel to explain their legal responsibilities.
Karen Roach, the association’s senior director of regulatory affairs and rural health, says the billing problem in New York doesn’t appear widespread.
“Some of these issues arose from greater automation of the billing process,” Roach says. “Training is needed to flag these cases, to put systems in place not to automatically generate a bill.”
Working with an advocacy group, Erin eventually got the hospital to stop billing her. But the emergency physicians group that treated her no longer exists, and her $131.68 bill has been bundled with other debts and resold to different collectors several times, she says.
When Erin tells a debt collector that the bill they’re calling about is for services related to rape, “They say, ‘Oh, we’ll fix it,’ but they don’t,” she says. “They just sell it again and it just becomes someone else’s problem. But it’s always my problem.”
Despite state and federal laws, many people who were raped wind up paying for some medical services out-of-pocket, even if they have insurance. An analysis of billing records from 1,355 insured female rape survivors found that in 2013 they paid an average $948 out-of-pocket for prescription drugs and hospital inpatient or outpatient services during the first 30 days after the assault. That amount represented 14% of total costs, the study found.
“We just assumed that this was only a problem for women who fell through the cracks,” says Kit Simpson, a professor in the department of health care leadership and management at the Medical University of South Carolina in Charleston, who co-authored the study. “But this was a systematic problem.”
Some people who have been assaulted sexually don’t want to use their insurance in any case, because they are worried about privacy or safety issues if family members or others find out, advocates say.
The Violence Against Women Act, often referred to as VAWA, is up for reauthorization this year. It’s not clear if a new bill would address these payment issues. If states don’t certify that they shoulder the cost of rape exams, funds can be frozen. (States must also certify that they don’t require these patients to participate in the criminal justice system.)
The Department of Justice declined multiple requests for comment on whether and how those VAWA provisions are enforced.
Some advocates for people who have been sexually assaulted would like to see the federal definition of what must be included in a no-cost medical forensic exam broadened to include such services as testing and medication for pregnancy and sexually transmitted infections, including HIV. Such a move would level the playing field across the U.S., they say.
Janine Zweig, associate vice president of justice policy at the Urban Institute, who co-authored a study examining state payment practices for rape exams, says a federal standard should be considered. “Do we really want it to be about which state you live in?”
Kaiser Health News is a nonprofit, editorially independent program of the Kaiser Family Foundation. KHN is not affiliated with Kaiser Permanente.
California First State To Offer Health Benefits To Adult Undocumented Immigrants

Gov. Gavin Newsom, left, talks with members of a Diabetes Talking Circle during his visit to the Sacramento Native American Health Center in Sacramento Tuesday.
Rich Pedroncelli/AP
hide caption
toggle caption
Rich Pedroncelli/AP
California has become the first state in the country to offer government-subsidized health benefits to young adults living in the U.S. illegally.
The measure signed by Gov. Gavin Newsom on Tuesday extends coverage to low-income, undocumented adults age 25 and younger for the state’s Medicaid program.
Since 2016, California has allowed children under 18 to receive taxpayer-backed healthcare despite immigration status. And state officials expect that the plan will cover roughly 90,000 people.
The idea of giving health benefits to undocumented immigrants is supported by most of the Democratic candidates running for president, and California’s move comes as the Trump administration continues to ramp up its hardline crackdown on unauthorized immigrants. On Tuesday, Newsom said the state law draws a sharp contrast with Trump’s immigration policies.
“If you believe in universal health care, you believe in universal health care,” Newsom said. “We are the most un-Trump state in America when it comes to health policy.”
In California, extending health benefits to undocumented immigrants is widely popular. A March survey conducted by the nonpartisan Public Policy Institute of California found that almost two-thirds of state residents support providing coverage to young adults who are not legally authorized to live in the country.
California, the institute notes, has more immigrants than any other state. And an estimated 14% of them are living in the state without legal status.
A national poll suggests that many Americans across the country are far less accepting of the notion of giving health coverage to those who came into the U.S. illegally. A CNN poll conducted after the Democratic debates last month found that 59% of those surveyed do not think government-backed health coverage should be provided to undocumented immigrants.
In most states, people living in the country illegally are not eligible for federal health insurance programs like Medicaid and Medicare, except is some cases, like medical emergencies and pregnancies, according to the National Conference of State Legislatures.
Republican lawmakers in California criticized the law, arguing that the state should be spending health care dollars on those living in the state legally.
“We are going to be a magnet that is going to further attract people to a state of California that’s willing to write a blank check to anyone that wants to come here,” said Republican Senator Jeff Stone at a May legislative hearing. “We are doing a disservice to citizens who legally call California their home.”
The plan does not cover all unauthorized immigrants under 25, only those whose incomes are low income to qualify. State officials estimate in the first year the program will cover around 138,000 residents and cost California taxpayers $98 million.
Trump has publicly attacked Newsom’s plans.
“It’s crazy what they’re doing. It’s crazy,” Trump told reporters last week. “And it’s mean, and it’s very unfair to our citizens. And we’re going to stop it, but we may need an election to stop it.”
The Affordable Care Act Is On Trial Again — This Time In Louisiana
Oral arguments wrapped up Tuesday in New Orleans in a closely-watched lawsuit that could eventually decide the fate of the Affordable Care Act.

